It takes, on average, 12 years and $2.6 billion to bring one drug to the market. Some 88% of drugs fail clinical trials and another 10% are withdrawn even after regulatory approval.
There are several reasons for this: One is that traditional pre-clinical testing models still rely on animals which can only go so far towards predicting the effects of an experimental medicine on the human body. The second is that if a drug fails in a clinical trial, it is necessary to go back to the beginning because it is impossible to know why it failed.
What’s more, even advanced technologies like artificial intelligence (AI), which have helped make major advances in the medical field such as genome sequencing have trouble to accurately read human biology.
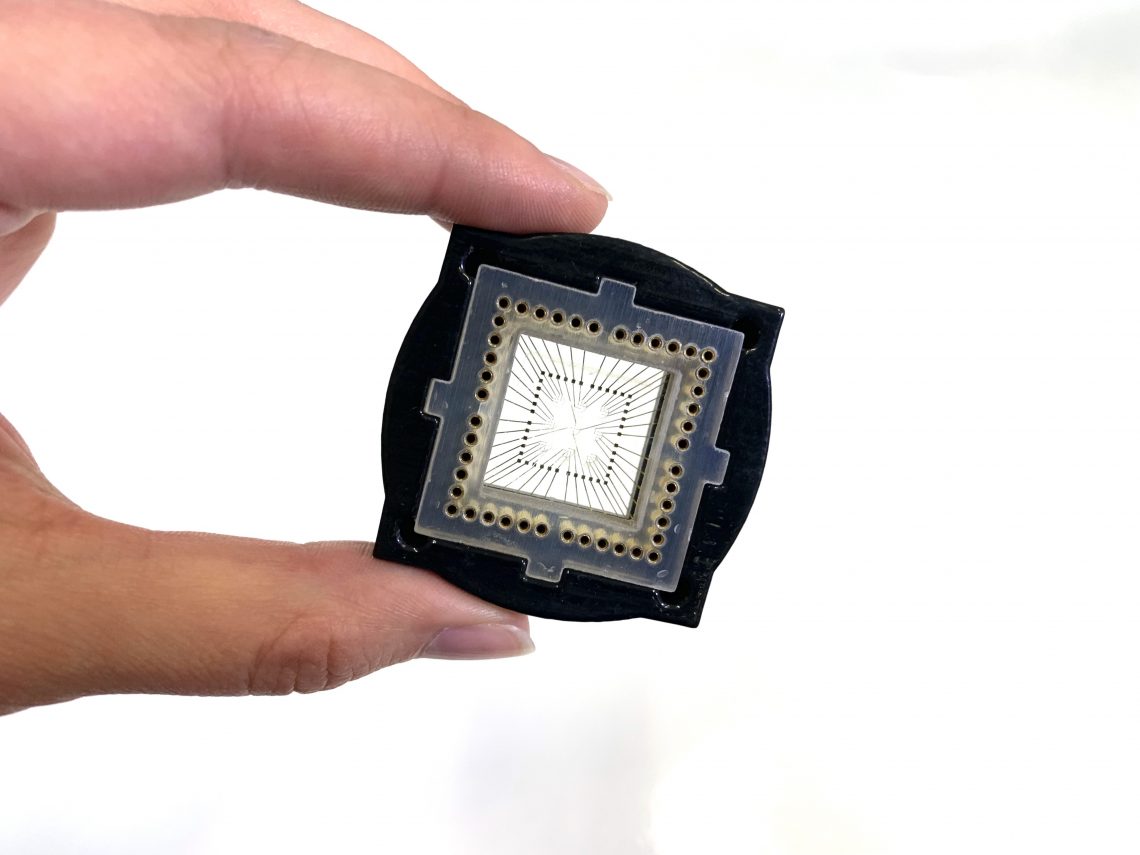
Tissue Dynamics, an Israeli startup spun out of the Alexander Grass Center for Bioengineering at the Hebrew University of Jerusalem, thinks it has found a way around these issues. It is harnessing AI and other cutting-edge technologies to test drugs on human tissue and detect potentially lethal side effects before drugs are prescribed to patients. The company was founded by Prof. Yaakov Nahmias, the director of Hebrew University’s Grass Center for Bioengineering, a faculty member at Harvard Medical School, a Fellow of the British Royal Society of Medicine and a serial entrepreneur. He is a recognized pioneer in the field of organs-on-chips, microfluidic devices that simulate the functions of living organs, more accurately reflecting human physiology than methods currently used in drug testing.
Organs-on-chips, which are poised to replace animal toxicity testing, offer a way to accelerate drug development and advance personalized medicine. The cosmetic, food and chemical industries also stand to benefit enormously from organ-on-chip technologies for both production and testing, as society seeks humanized in vitro alternatives to animal testing, according to a May 12 article in Nature.
Nahmias not only established the core technology for the first organ-on-a-chip company on the market from his laboratory at Harvard Medical School in 2009, he was also the first to insert optoelectronic sensors inside human living tissues on chips, creating tiny bionic organs such as hearts, brains, livers, and kidneys, that can output useful real-time data about human biology’s reaction to drugs. The technology was established in Jerusalem in 2015. Since then, he and his team of researchers at Hebrew University have demonstrated that if organs-on-a-chip are equipped with integrated sensors it is possible to monitor metabolic functions of cells exposed to different drug concentrations over a long period of time. The approach permits detection of drug efficacy or toxicity before any effects on cell or tissue viability or function can be observed using traditional methods.
For example, Nahmias and his team used human liver tissue on a chip to study troglitazone (Rezulin), which was used to treat type-2 diabetes until it was removed from the market after it was found to induce severe liver injury in 1 out of every 30,000 patients. The drug cost the manufacturer more than $750 million in lawsuits. The Hebrew University’s liver-on-chip technology detected mitochondrial stress, which is an early sign of undetected cellular damage. If the manufacturer had access to this liver-on-chip technology, instead of traditional drug testing, Nahmias says the company would have been alerted to this side effect and could have made tweaks to the drug before it was put on the market.
Nahmias now wants Tissue Dynamics to take things to the next level by using a robotic platform that can simultaneously handle 19,000 sensor-equipped human micro organs. This robotic system is being designed to autonomously make the organs-on-chips, test molecules that are applied to them, identify the ones that work, do safety assessments, and produce final drug treatments using AI-based tools. The technology received the European Seal of Excellence in 2021 and Tissue Dynamics was recently selected as one of the top five emerging organ-on-chip companies in the world.
If it works and the process scales “we think we can reduce the cost of drug development by over 75% from $2.6 billion to half a billion dollars per drug,” says Nahmias, who was interviewed live on stage at DLD, a conference in Munich May 20-22, by The Innovator’s Editor-in-Chief.
NEXT GEN ORGANS-ON-CHIPS
Organs-on-chips were selected in 2016 as one of the top ten emerging technologies by the World Economic Forum. Today dozens of companies produce them, but their approaches vary widely. Some, like Nortis and MIMETAS, sell chips for use in laboratories that allow the placement of human cells in different chambers, helping improve methods for preclinical pharmacology and toxicology studies. For example, MIMETAS is a partner in the Oncode-PACT (Preclinical Accelerator for Cancer Treatments) initiative that on April 14 was granted €325 million by the Dutch National Growth Fund to develop cancer drug candidates faster and bring them to patients sooner. As a partner in Oncode-PACT, MIMETAS will develop the next generation of patient-specific cancer organoid models that include immune cells, blood vessels, and other essential cell types to drive novel cancer drug discovery and development. Using these models, MIMETAS says it will screen compounds and targets using fully integrated, automatic phenotypic screening lines with AI data interpretation, bringing early validation and de-risking to the cancer drug development pipeline.
A Boston-based company called Emulate, which in March was named one of 15 companies that promise to transform the medtech industry by industry publication Fierce BioTech, is taking a different approach. It makes a kit that researchers can use to create their own specialized tissue experiments but also offers six self-contained organ chips, mimicking the brain, heart, kidney, liver, lungs, and small and large intestines.
Emulate, which has originally formed around technology developed at Harvard University’s Wyss Institute for Biologically Inspired Engineering, made headlines in May with its new colon-intestine chip, which it says enables the most human-relevant preclinical assessment of inflammatory bowel disease (IBD) drug candidates, helping researchers to safely test out potential new therapies that are designed to interact with immune cells and guide their actions before committing to full clinical trials.
Another category of organ-on-a-chip makers develops highly customized 3D human tissues to advance drug development. One of them, a Swiss company called InSphero, launched a pre-competitive consortium in June of last year that brings together representatives from pharmaceutical companies engaged in the development of cross-species drug testing and validation strategies for rapid, reliable drug-testing of drug-induced liver injury. Another company in this category, San Diego, California-based Organovo is using one of its 3D models to attempt to mimic the architecture, cell diversity, and function of the human gut in healthy and disease states. Organova announced in May that it believes that its first IBD model correctly demonstrates key aspects of Crohn’s patient biology that differ from a non-diseased state, and that this finding can be used to find and characterize therapeutics.
Nahmias says Tissue Dynamics, which is currently raising a Series A round of funding, will go further than existing organ-on-chip companies, taking Next-Gen chips to the next level. “Our DynamiX platform uses sensors to detect tissue activity in real time; our software is able to detect mechanism of action, we have 3D models of the liver, heart, brain and kidneys; we integrate our tissue models with sensors in a single robotic platform that can run over 19,000 tissues at once; and we use machine learning tools to develop drugs,” he says.
IMPROVING TREATMENTS FOR EVERYTHING FROM COVID TO CANCER
Even before adding the robotic platform it is building with the help of Beckman Coulter, a company that develop products that automate complex biomedical testing, the technology used by Tissue Dynamics has been able to demonstrate the potential of AI- powered organ-on-chip technology to advance medical treatments, says Nahmias.
For example, in June 2020 Nahmias and his team announced that their experiments indicated that fenofibrate, a cheap and common drug, could help coronavirus patients. The lab charted the metabolic response of lung epithelial cells to SARS-CoV-2 infection both on organ-on-a-chip primary cultures and COVID-19 patient samples. Analysis of human tissue on a chip showed that viral replication induces lipid accumulation in the lungs. Metabolism-focused drug screening using advance software tools showed that fenofibrate can reverse lipid accumulation and block SARS-CoV-2 replication. Analysis of 3,233 Israeli patients hospitalized due to COVID-19 supported the in vitro findings. Patients taking fibrates showed significantly lower markers of immunoinflammation and faster recovery. Abbott Laboratories, one of several manufacturers of fenofibrate, provided a grant to support the research. While small patient cohort showed promising results, the randomized placebo controled clinical study will only be complete this August.
The technology Nahmias and his team have developed is also credited with improving treatment for cancer patients.
Using a kidney-specific tissue-on-a-chip technology, researchers from Hebrew University and Tissue Dynamics uncovered the mechanism that causes kidney damage from the widely used chemotherapy drug – cisplatin, as well as a treatment to prevent or reverse the damage. Using human tissue cells in a microfluidic environment that mimics the function of the kidney proximal tubule—a structure that is particularly sensitive to drug toxicity and often the site of the kidney’s first and most severe damage from nephrotoxic therapies—the team embedded biosensors to track the tissue’s response to drugs in real time.
The study, which was published on the cover of Science Translational Medicine, found that the anti-cancer drug cisplatin caused kidney cells to accumulate too much sugar. The solution was to add a drug that blocked this sugar reabsorption, and essentially eliminated the nephrotoxic effect of this chemotherapy treatment. Analysis of 247 Israeli patients taking nephrotoxic drugs supported the in vitro findings. Thanks to its discovery, cancer patients can receive higher doses of cisplatin for longer durations of treatment without the side effects associated with chemo, he says.
A NEW ERA FOR DRUG DEVELOPMENT
Nahmias says the technology used by Tissue Dynamics helps researchers understand human biology in ways that would have been impossible until now, even with state-of-the-art AI systems costing tens of millions of dollars. What works well for a rodent in animal tests may not work in a human body, or worse, be toxic. By eliminating animal testing and instead working directly on human tissue with embedded sensors, drugs can be tested more quickly and accurately, he says. He likens Tissue Dynamics technology to a car dashboard that lights up when something starts to go wrong. “Sensors in our cars, changed the way we drive. Now we can do the same for the human body and for the first time understand why a drug doesn’t work or how it might do harm,” he says.
And, just like the next level in cars is autonomous driving, he believes automized organs-on-chips testing will be the Next Big Thing in drug discovery, transforming the pharma industry. That’s why Tissue Dynamics is adding robotics into the mix, a move that it says it believes will significantly slash the cost of developing drugs.
“Today thousands of small pharma companies are developing drugs but all of them need to be sold to mega corporations to support what is needed for Phase III trials,” says Nahmias. “If we can dramatically reduce the cost and risk of drug development by allowing intelligent robotic systems to interact with human biology on chip, we will go beyond a few pharmaceutical giants and greatly expand the field for thousands of companies. It will completely change the ecosystem and we can start thinking about treating orphan diseases, initiating massive repurposing efforts to treat diseases in sub-Saharan Africa or developing specific personalized medicine in areas where speed is really of the essence. This is the vision of Tissue Dynamics and it could be transformative.”
This article is content that would normally only be available to subscribers. Sign up for a four-week free trial to see what you have been missing.